
The National Institutes of Health’s National Center for Advancing Translational Sciences (NCATS) was established to transform the translational process so that new treatments and cures for disease can be delivered to patients faster. ASHG recently spoke with Joni L. Rutter, PhD, Director of NCATS, about how human genetics and genomics is fueling the translational pipeline by turning observations in the laboratory, clinic, and community into interventions that improve the health of individuals and the public, from diagnostics and therapeutics to medical procedures and behavioral changes.
What is the unique role of the National Center for Advancing Translational Sciences (NCATS) and how does it engage with human genetics and genomics specifically?
The National Center for Advancing Translational Sciences (NCATS) plays a pivotal role in transforming translational science to accelerate the journey from research to health impact.
Founded 12 years ago, our mission is to expedite the translation of scientific discoveries into tangible health solutions. NCATS uniquely intervenes at every stage of the translational journey, from understanding the biological and chemical foundations of potential disease targets to implementing clinical strategies that enhance health outcomes. Our strength lies in overcoming major translational obstacles, whether they be scientific, operational, or administrative, thereby catalyzing progress across diverse research areas and diseases.
While our scope is broad, we place a special emphasis on rare diseases, approximately 80% of which are genetically rooted. By leveraging advancements in diagnostics and gene targeted therapies, such as gene therapy and gene editing, we want to enable the development of curative treatments, particularly for rare genetic disorders.
Given that not all diseases or conditions have a known treatment and drug development can take decades, how does NCATS help speed the development of therapies or novel applications of existing drugs?
Only 5% of rare diseases have therapies. A core goal of NCATS is to address the daunting challenge of developing treatments for these disorders, which number more than 10,000. NCATS employs a multi-faceted, platform-based strategy to tackle these challenges simultaneously across multiple diseases. For instance, the Rare Diseases Clinical Research Network (RDCRN) enables the study of multiple rare diseases concurrently, enhancing our efficiency and understanding of diseases with common biology or features. Our collaboration with 10 different NIH institutes and centers amplifies the reach and effectiveness of this network.
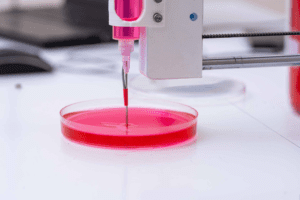
Other NCATS programs highlight and leverage technological innovations. We develop and hone cutting-edge technologies like 3-D tissue bioprinting and tissue chips, which offer more accurate models of human physiology. These tools are pivotal in predicting drug toxicity and efficacy, which promise to streamline the drug development process. Bridging data silos is a necessary task, and NCATS has invested heavily in organizing, aggregating, and harmonizing quality data and making them available openly and responsibly. Our commitment to data science and informatics, including the application of artificial intelligence/machine learning (AI/ML) algorithms, underpins all our programs. This approach is crucial for the design of novel bioactive molecules and in drug repurposing, where we identify new applications for existing drugs.
The Clinical and Translational Science Awards (CTSA) Program is another cornerstone of our strategy. It fosters a national network of medical institutions dedicated to swiftly translating research discoveries into improved patient care.
What kind of collaborations does NCATS support across scientific disciplines and organizations?
At NCATS, the ‘T’ not only stands for Translational but also for ‘Team’, embodying our belief that Translational Science thrives on team science.

I’ve mentioned our more-than-one-disease-at-a-time approach, but when there is a specific disease with a potential therapeutic path, NCATS’ intramural Therapeutics for Rare and Neglected Diseases (TRND) and extramural Drug Development Partnerships Program (ODDPP) programs epitomize this spirit of fostering therapeutic development partnerships across NIH, academia, nonprofits, and industry. Leveraging our resources, such as our 370,000 compound library and our expertise, we guide therapeutics from the lab through preclinical testing and the U.S. Food and Drug Administration (FDA) Investigational New Drug application processes, effectively ‘de-risking’ candidates for external partners and clinical trial planning.
A prime example is our response to the COVID-19 pandemic through the National COVID Cohort Collaborative (N3C). This CTSA-led partnership brought together a wide array of partners to analyze real-time clinical data, enhancing our understanding and treatment strategies for COVID-19. The success hinged on seamlessly integrating deidentified electronic health record data with other data sources and a collaborative analytics framework, enabling an interdisciplinary team of experts to access and analyze over 21 million records, linked with Centers for Medicare and Medicaid data, vaccination, and other data types. This herculean effort across the scientific community, including a significant partnership with the National Institute of General Medical Sciences IDeA network, underscores our commitment to collaborative science.
What is the role of NCATS in developing gene therapies for both rare and common diseases? How does NCATS aim to make gene therapy development and clinical testing more streamlined, more efficient, and potentially more accessible?
This is an area of great excitement at NCATS. We’re actively involved in key initiatives like the Somatic Cell Genome Editing (SCGE) program, the Accelerated Medicines Partnership – Bespoke Gene Therapy Consortium (BGTC), and the Platform Vector Gene Therapy project (PaVe-GT). In the latter, our collaboration with the National Human Genome Research Institute, the National Institute of Neurological Disorders and Stroke, and the NIH Clinical Center is propelling the project towards its first clinical trial within the next 18 months. The project recently received orphan drug and rare pediatric disease designations from the FDA. NCATS also provides templates of the PaVe-GT model for others who are developing gene therapies.
The cornerstone of these programs is the innovation in gene therapy delivery methods. We’re enhancing the understanding of viral vectors, refining manufacturing processes for gene delivery systems, and streamlining regulatory pathways from preclinical to clinical stages.
Our focus extends beyond AAV-based therapies, tackling shared challenges in gene editing technologies like CRISPR-Cas9. These include targeted delivery, immune response management, and cell-specific targeting. The efficiencies we achieve here have broader implications, potentially revolutionizing precision medicine, ‘N-of-1’ trials and offering new avenues for treating more common diseases.
Inclusion of populations from diverse ancestries in studies is revealing novel insights about drug responses, diagnostic accuracy, and disease risk. How is NCATS working to increase the diversity of research cohorts as well as diversity in clinical trials?
Inclusion is central to our vision of getting more treatments for all people more quickly. Genetics, lifestyle, and other factors play an important role in health disparities and interact in complex ways. We are working to bring these factors to the forefront of our research planning, design, and implementation so all can benefit from the results. For example, NCATS is creating a health equity lens for evaluating the generalizability of preclinical human cell-based models, such as tissue chips and 3D bioprinted cells, for drug development.
 Some key examples of how we support inclusivity are by innovating in ways we engage and work with patient organizations through the RDCRN Patient Advocacy Groups and with communities through our CTSA Trial Innovation Network. Having patients, patient advocates, and community voices at the table helps ensure that our research and development efforts are scientifically sound and also aligned with the actual needs and experiences of those we aim to help.
Some key examples of how we support inclusivity are by innovating in ways we engage and work with patient organizations through the RDCRN Patient Advocacy Groups and with communities through our CTSA Trial Innovation Network. Having patients, patient advocates, and community voices at the table helps ensure that our research and development efforts are scientifically sound and also aligned with the actual needs and experiences of those we aim to help.
Another focus area for us is creating more on-ramps into the translational science workforce. Training and education across all career stages, the earlier the better, is integral to this success. We have a variety of programs to support these activities, including diversity supplements.
What are some of the goals and aspirations for NCATS in the coming years? What most excites you about opportunities for human genetics to improve medicine?
In the early stages of my career, I was deeply involved in gene hunting and Genome-Wide Association Studies (GWAS). This work was thrilling as we identified genes linked to various diseases, but it often felt like a half-completed puzzle. We celebrated each discovery, yet the next step – translating these findings into treatments – remained elusive.
Today, at NCATS, we’re actively seeking ways for genetics to tell us more about diagnostics and targeting these genes for therapeutic interventions.
A particularly exciting and needful frontier is newborn screening, where we are working to challenge traditional diagnostic approaches. The current rare disease diagnostic journey, averaging 6-8 years, is too long and can deny patients timely access to life-altering therapies. Our goal is to develop a path for a ‘sequence-first’ approach in high-risk infants, using whole genome sequencing not just as a tool for diagnosis but as a proactive strategy in medical care. While individual disorder incidence might be low, collectively, this approach has the potential to transform outcomes for thousands of babies annually. By breaking down the barriers of cost and access to whole genome sequencing, the genomics community is poised to redefine the landscape of early disease detection, with breakthrough interventions promising to be real options.
NCATS is actively developing our strategic plan for 2024-2029. This plan will be a roadmap for shaping the advancements in translational science. I invite the ASHG community to explore our strategic framework and join us in pushing the boundaries of what’s possible at the intersection of genetics and translational science: NCATS 2024-2029 Strategic Plan.
For more information about NCATS, see https://ncats.nih.gov/.
